Advancing Mental Healthcare in India

| “India’s vision of good health implies not just being free of disease but to ensure wellness and welfare for everyone. The goal is to ensure physical, mental and social wellbeing.” Shri Narendra Modi, Prime Minister of India |
What is Mental Health
Mental health refers to an individual’s emotional, psychological, and social well-being. It influences how people think, feel, and behave in daily life. It also affects decision-making, stress management, and relationships. According to the World Health Organization (WHO), mental health is a state of mental well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community.
Impact of Poor Mental Health
- Impact on Productivity: Poor mental health leads to lower workplace performance, increased absenteeism, and reduced efficiency.
- Social and Emotional Well-being: Mental well-being affects interpersonal relationships, self-confidence, and social interactions.
- Economic Impact: According to WHO, mental disorders contribute significantly to the global burden of disease, and untreated conditions can lead to high economic costs.
Mental Health Scenario in India
- WHO Data Insight
- India contributes to 18% of the global population. WHO estimates that the burden of mental health problems in India is 2443 disability-adjusted life years (DALYs) per 10000 population; the age-adjusted suicide rate per 100000 population is 21.1. The economic loss due to mental health conditions, between 2012-2030, is estimated at USD 1.03 trillion.
- Prevalence:
- The National Mental Health Survey (NMHS) 2015-16 by NIMHANS found that 10.6% of adults in India suffer from mental disorders.
- The lifetime prevalence of mental disorders in India is 13.7%.
- National studies reveal that 15% of India’s adult population experiences mental health issues requiring intervention.
- Urban areas have a higher prevalence (13.5%) compared to rural (6.9%).
- Treatment Gap
- 70% to 92% of people with mental disorders do not receive proper treatment due to lack of awareness, stigma, and shortage of professionals.
- According to the Indian Journal of Psychiatry India has 0.75 psychiatrists per 100,000 people, whereas WHO recommends at least 3 per 100,000.
Insights from Economic Survey 2024-25
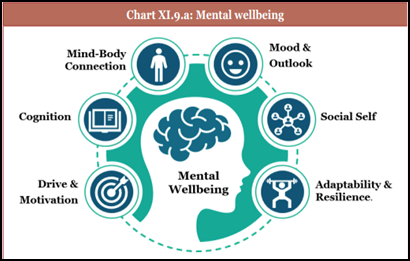
Mental wellbeing is the ability to navigate life’s challenges and function productively. Recognising its importance, Economic Survey 2024-25 highlighted that Mental well-being encompasses all our mental-emotional, social, cognitive, and physical capabilities. This can also be construed as the mind’s composite health. It emphasised a whole of community approach to tackling mental health problems and stated that it is about time to find viable, impactful preventive strategies and interventions. India’s demographic dividend is riding on skills, education, physical health and, above all, mental health of its youth.
The Economic Survey 2024-25 suggested:
- Enhance Mental Health Education in Schools: Early intervention strategies to address anxiety, stress, and behavioural issues in students.
- Improve Workplace Mental Health Policies: Address job stress, long working hours, and burnout.
- Expand Digital Mental Health Services: Strengthen Tele MANAS and integrate AI-based mental health solutions.
Mental Health Infrastructure in India
- As part of the National Mental Health Programme, in 2024, 25 Centres of Excellence were sanctioned set up to train more postgraduate students in mental health and provide advanced treatment.
- 47 PG Departments in mental health have been established or upgraded in 19 government medical colleges. Mental health services are also being introduced in 22 newly established AIIMS.
- 47 Government-Run Mental Hospitals including 3 Central Mental Health Institutions, viz. National Institute of Mental Health and Neuro Sciences, Bengaluru, Lokopriya Gopinath Bordoloi Regional Institute of Mental Health, Tezpur, Assam and Central Institute of Psychiatry, Ranchi.
- Integration of Mental Health Services in Ayushman Bharat – Health & Wellness Centres (HWCs)
Under Ayushman Bharat, the government has upgraded more than 1.73 lakh Sub Health Centres (SHCs) and Primary Health Centres (PHCs) to Ayushman Arogya Mandirs. Mental health services have been added in the package of services under Comprehensive Primary Health Care provided at these Ayushman Arogya Mandirs. These HWCs provide:
- Basic counselling and psychiatric medication at PHC levels.
- Training for general physicians to handle mild-to-moderate mental health conditions.
- Linkages to district hospitals for advanced psychiatric care.
This initiative ensures that mental healthcare is available in both urban and rural areas, reducing dependence on specialized hospitals and making psychiatric care more community-centric.
Policies and Schemes Undertaken by the Government of India
National Mental Health Programme (NMHP) – 1982
Recognizing the growing burden of mental disorders and the shortage of mental health services, India launched the National Mental Health Programme (NMHP) in 1982. The primary goal was to ensure that mental healthcare becomes an integral part of the general healthcare system, rather than being confined to specialized hospitals.
Key components include:
District Mental Health Programme (DMHP)wasintroduced under NMHP to expand community mental health services.
- Covers 767 districts
- Provides counselling, outpatient services, suicide prevention programs, and awareness initiatives.
- 10-bedded inpatient mental health facilities at the district level.
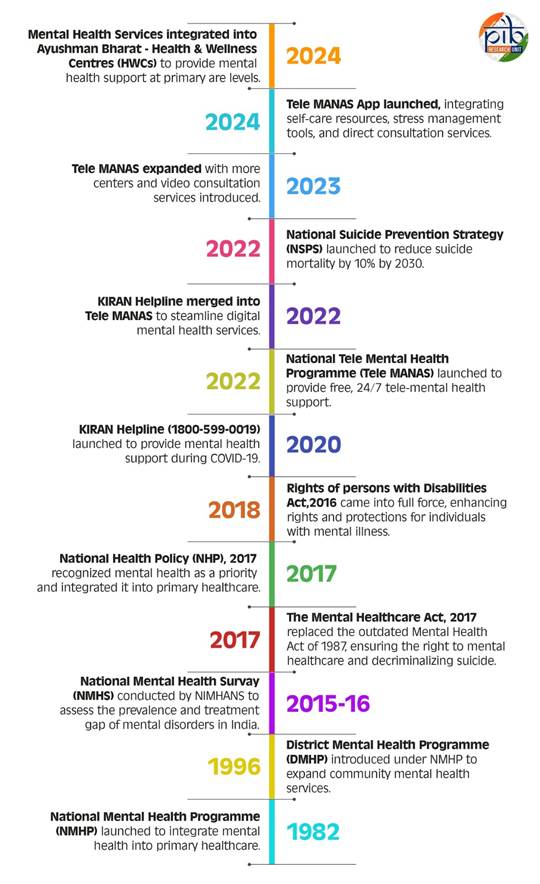
NIMHANS Act, 2012
The NIMHANS Act, 2012, was a significant step towards enhancing mental health education and research in India. Under this act, the National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru, was declared an Institute of National Importance. This recognition allowed NIMHANS to expand its academic and research capabilities, making it the premier institution for psychiatry, neuropsychology, and mental health sciences in India.
The Rights of Persons with Disabilities (RPwD) Act, 2016
The Rights of Persons with Disabilities (RPwD) Act which replaced the Persons with Disabilities (PWD) Act, 1995, expanded the definition of disability to include mental illness and introduced stronger legal protections for individuals with psychosocial disabilities. The Act aligns with India’s commitment to the UN Convention on the Rights of Persons with Disabilities (UNCRPD) and aims to ensure equality, dignity, and non-discrimination for persons with disabilities, including those with mental health conditions.
National Mental Healthcare Act, 2017
The Mental Healthcare Act, 2017, was enacted to ensure the right to mental healthcare services, protect the dignity and rights of individuals with mental illness, and align India’s mental health laws with international standards, particularly the United Nations Convention on the Rights of Persons with Disabilities (UNCRPD). The Act replaced the Mental Health Act of 1987 and introduced several progressive changes to mental health care and services in India like the Right to affordable and quality mental healthcare services and the decriminalization of suicide in India.
National Health Policy, 2017
The National Health Policy (NHP), 2017 was a landmark that acknowledged mental health as a national health priority. This policy aimed to address mental health issues through a multi-pronged approach, integrating mental healthcare into primary healthcare, strengthening human resources, and improving treatment accessibility.
By placing mental health at the center of India’s healthcare framework, NHP 2017 aimed to bridge the treatment gap by making psychological services available at Primary Health Centres (PHCs) and Health and Wellness Centres (HWCs) under Ayushman Bharat.
iGOT-Diksha Collaboration for Mental Health Training
The government has also collaborated with the iGOT-Diksha platform, a digital learning initiative in 2020, to train healthcare professionals, frontline workers, and community health volunteers in mental healthcare. This program focuses on:
- Building capacity for mental health care at the grassroots level.
- Equipping doctors and nurses with skills to diagnose and treat mental disorders.
- Promoting mental health awareness in rural areas.
Through iGOT-Diksha, India has expanded its mental health workforce, ensuring better early intervention strategies and community support mechanisms.
National Tele Mental Health Programme (Tele MANAS), 2022
Launched on October 10, 2022, the National Tele Mental Health Programme (Tele MANAS) was a game-changer in India’s digital mental health infrastructure. Tele MANAS provides free, 24/7 mental health support to individuals through a national toll-free helpline (14416 / 1800-89-14416). Available in 20 Indian languages.
As of February 7, 2025, the Tele MANAS helpline has handled over 1.81 million (18,27,951) calls since its launch in 2022, providing essential mental health support across India. There are 53 Tele MANAS Cells across various states, ensuring local access to mental health services. The program is supported by 23 Mentoring Institutes nationwide, along with 5 Regional Coordinating Centers, ensuring efficient service delivery and expert guidance in mental healthcare.
Tele MANAS services include:
- Immediate tele-counselling by trained professionals.
- Referral support to psychiatrists for severe cases.
- Mental health awareness campaigns via digital platforms.
- Mobile-based mental health interventions, ensuring accessibility in rural and remote areas.
Tele MANAS Mobile App & Video Consultation
- The Tele MANAS App was launched in October 2024.
- Offers self-care strategies, stress management tools, and direct access to mental health professionals.
- Video consultation services introduced in Karnataka, Tamil Nadu, and J&K.
WHO Recognition
The World Health Organization (WHO) praised Tele MANAS as an effective and scalable mental health solution, making mental healthcare more inclusive and affordable.

KIRAN Helpline Merged into Tele MANAS
The KIRAN Helpline (1800-599-0019), initially launched in 2020, was merged into Tele MANAS in 2022 to enhance the efficiency of mental health support services. This transition streamlined mental health helpline operations, making it more accessible and better integrated with India’s healthcare system.
During COVID-19, the government took crucial steps to support mental health. A 24/7 helpline provided nationwide psychosocial assistance, while health workers received online training through the iGOT-Diksha platform. Public awareness campaigns spread stress management strategies via media, and official guidelines and advisories were issued to promote mental well-being. These interventions played a vital role in addressing the psychological challenges of the pandemic.
National Suicide Prevention Strategy, 2022
The National Suicide Prevention Strategy (NSPS) was launched by the Ministry of Health and Family Welfare (MoHFW) in 2022, with the goal of reducing suicide mortality by 10% by 2030. Recognizing suicide as a public health concern, the strategy focuses on early intervention, crisis management, and mental health promotion.
Key components of NSPS include:
- Mental health screenings for students in schools and colleges.
- Establishing crisis helplines and psychological support centers.
- Community awareness programs to break the stigma around mental illness and suicide.
- Stronger implementation of workplace mental health programs.
By focusing on high-risk populations, such as students, farmers, and young adults, the strategy ensures targeted intervention to prevent self-harm and improve overall well-being.
Conclusion
India has made notable progress in mental healthcare through policy reforms, digital initiatives like Tele MANAS and expanding access to services under programs such as NMHP, Ayushman Bharat HWCs, and the National Suicide Prevention Strategy. Moving forward, India must strengthen awareness campaigns, expand workforce training and invest in digital mental health solutions. A mentally healthier India is vital for individual well-being, economic growth, and national development, requiring a whole-of-society approach to make mental healthcare accessible, inclusive, and stigma-free.
References
- https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1919922
- https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
- https://pib.gov.in/PressReleaseIframePage.aspx?PRID=2034931
- https://www.who.int/health-topics/mental-health#tab=tab_2
- National Mental Health Survey, 2015-16 – Summary Report_0.pdf
- https://pib.gov.in/PressNoteDetails.aspx?NoteId=153277&ModuleId=3®=3&lang=1
- https://sansad.in/getFile/rsnew/Committee_site/Committee_File/ReportFile/14/187/148_2023_9_17.pdf?source=rajyasabha
- https://www.who.int/india/health-topics/mental-health
- https://mohfw.gov.in/?q=pressrelease-40
- https://pib.gov.in/PressReleaseIframePage.aspx?PRID=2043511#:~:text=Besides%20the%20above%2C%20the%20Government,started%20tele%20mental%20health%20services
- https://mohfw.gov.in/sites/default/files/9903463892NMHP%20detail_0_2.pdf
- https://pib.gov.in/PressReleasePage.aspx?PRID=2043511#:~:text=The%20District%20Mental%20Health%20Programme,prevention%20services%2C%20work%20place%20stress
- https://nimhans.co.in/about-us/
- https://nhrc.nic.in/sites/default/files/DisabilityRights.pdf
- https://mohfw.gov.in/sites/default/files/9147562941489753121.pdf
- https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1513000
- https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1612437
- https://pib.gov.in/PressNoteDetails.aspx?NoteId=153277&ModuleId=3®=3&lang=1
- https://telemanas.mohfw.gov.in/telemanas-dashboard/
- https://www.indiabudget.gov.in/economicsurvey/doc/eschapter/echap11.pdf
- https://pib.gov.in/PressReleaseIframePage.aspx?PRID=2006265#:~:text=On%20this%20occasion%2C%20Dr%20Paul,the%20concerned%20persons%20with%20ease%E2%80%9D.
- LOK SABHA UNSTARRED QUESTION NO. 1507, Lok Sabha 2023
- https://pib.gov.in/PressReleasePage.aspx?PRID=2097865
- https://mohfw.gov.in/sites/default/files/Mental%20Healthcare%20Act%2C%202017_0.pdf
****
Santosh Kumar / Sarla Meena / Vatsla Srivastava
(Release ID :267158)